Laparoscopic Cholecystectomy
Laparoscopic Gastrectomy
Laparoscopic Cholecystectomy
Laparoscopic Cholecystectomy
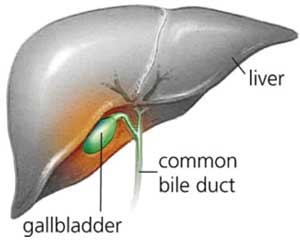 Many patients have gallstones which do not cause symptoms and require no surgery. If, however, these stones attempt to pass out of the gallbladder and block the gallbladder outlet, severe upper abdominal pain can develop.
Many patients have gallstones which do not cause symptoms and require no surgery. If, however, these stones attempt to pass out of the gallbladder and block the gallbladder outlet, severe upper abdominal pain can develop.
Common symptoms may include:
- Upper abdominal pain, occurring after meals rich in fat.
- Nausea and vomiting.
- Pain between the shoulder blades, and beneath the right shoulder.
- Chills and fever.
- Symptoms usually last for short periods of time and often occurs after fatty meals which stimulate the gallbladder to contract.
The formation of gallstones seems to be related to many factors, some of which are:
- Body weight - over-weight people have a higher incidence of gallstones.
- Diet - a diet high in fat and cholesterol, and low in fibre.
- Gallbladder motility - if the gall bladder is slow to drain.
- Rapid weight loss - bariatric surgery patients experience higher incidences of gallstones.
Acute Cholecistitis
Occasionally, these stones may become lodged within the neck of the gallbladder and result in prolonged episodes of pain associated with infection. This is known as acute cholesystitis and generally requires admission to hospital and cholecystectomy.
Obstructive Jaundice
Another complication of gallstones may be obstructive jaundice. In this situation, the gallstones pass out of the gallbladder and into the bile duct where they block the bile duct exit; that is, the gallstones prevent the flow of bile secretions into the duodenum. Jaundice is first recognised in the eyes, but acute jaundice results in a yellow tinge onto the skin. This may result in cholangitis, a progressive form of jaundice and infections. This needs to be treated immediately. Once a person has had one attack of gallstones, they are likely to develop more. It is thus wise to remove the gallbladder between attacks, since surgery is simpler when there is no acute infection or obstruction.
Treatment
A small hole (port) is created, in the belly button, followed by the insertion of a thin scope with a camera at its end to allow visualisation within the abdominal cavity. A second port is placed just under the breast bone, sternum, in the mid line of the abdomen, while third and fourth ports are placed in the right side of the abdomen. (These allow for removal of the gallbladder later in the procedure.).
The gallbladder is then freed of any scar tissue which may be present from previous episodes of acute cholecystitis. The cystic duct (the duct that joins the gallbladder to the bile duct) is then identified. Also identified is the cystic artery, a small blood vessel leading to the gallbladder.
The cystic duct is divided after sealing it with metallic clips. The cystic artery is then clipped and divided and the gallbladder is separated from the bed of the liver with a cautery device or laser. The gallbladder is then removed through one of the small incision ports. Finally, the ports are closed.
Patients are able to eat immediately after waking from a lap chole procedure and are usually discharged home the next day. Most patients return to normal activities within one to two weeks of their surgery.
The gallbladder is then freed of any scar tissue which may be present from previous episodes of acute cholecystitis. The cystic duct (the duct that joins the gallbladder to the bile duct) is then identified. Also identified is the cystic artery, a small blood vessel leading to the gallbladder.
The cystic duct is divided after sealing it with metallic clips. The cystic artery is then clipped and divided and the gallbladder is separated from the bed of the liver with a cautery device or laser. The gallbladder is then removed through one of the small incision ports. Finally, the ports are closed.
Patients are able to eat immediately after waking from a lap chole procedure and are usually discharged home the next day. Most patients return to normal activities within one to two weeks of their surgery.
Complications
Laparoscopic cholecystectomy has a complication rate of under two percent. It is a well-documented and frequently-performed procedure. Most patients recover and resume normal activities quickly. Rarely does the surgery impact adjacent organs in the body. When this occurs, a second procedure may be required.
Laparoscopic Gastrectomy
Laparoscopic Gastrectomy
Overview
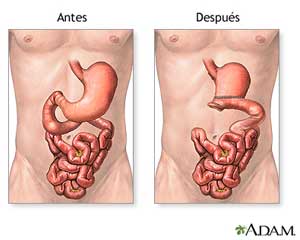 A gastrectomy is a procedure done to remove part or all of the stomach. When done using "keyhole" surgery it is called a laparoscopic gastrectomy. While the stomach is part of the digestive tract, with several lifestyle changes and the assistance of your doctors, you can still digest liquids and foods.
A gastrectomy is a procedure done to remove part or all of the stomach. When done using "keyhole" surgery it is called a laparoscopic gastrectomy. While the stomach is part of the digestive tract, with several lifestyle changes and the assistance of your doctors, you can still digest liquids and foods.
Indications
A laparoscopic gastrectomy is generally done as treatment for cancerous tumours in the stomach but may also be done to remove polyps, or growths inside your stomach or to treat severe stomach ulcers. There are three major types of gastrectomies: partial, complete and sleeve gastrectomies. Which of the above-mentioned types chosen by your surgeon will depend on your particular case.
What happens during a laparoscopic gastrectomy?
Under general anaesthesia a few small incisions will be made in the abdomen. Through these incisions a laparoscope, which is a thin surgical tool fitted with a camera and light, will be inserted. This provides your surgeon with images of the internal structures without the need for a larger incision. With this visualisation, Dr Heyns can remove part (a partial gastrectomy) or all (a complete gastrectomy) of the stomach as well as some nearby tissue like your lymph nodes.
Thereafter, depending on your specific case, your digestive tract will be rebuild accordingly. If a partial gastrectomy was done, the remaining part of your stomach will be connected to your bowel. If the entire stomach was removed your esophagus will be connected directly to your small intestine.
While Dr Heyns prefers the least invasive approach, this surgery can also be done through traditional open surgery.
Thereafter, depending on your specific case, your digestive tract will be rebuild accordingly. If a partial gastrectomy was done, the remaining part of your stomach will be connected to your bowel. If the entire stomach was removed your esophagus will be connected directly to your small intestine.
While Dr Heyns prefers the least invasive approach, this surgery can also be done through traditional open surgery.
What to expect after surgery
You can expect to stay in the hospital for one to two weeks after the surgery. While in hospital you will be fed through a tube in your vein until you are able to eat normally. Various lifestyle and dietary changes may need to be made but your doctor will discuss this with you prior to surgery. A dietician will then discuss your restrictions with food after surgery. Since laparoscopic surgery is less painful and allows for a quicker recovery time, you can expect to be back to your normal day-to-day routine in 3 weeks.
Click on the sections here above for more details
Laparoscopic Cholecystectomy
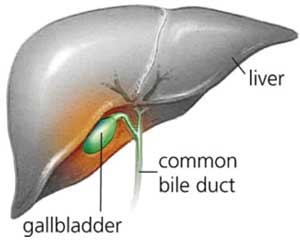 Many patients have gallstones which do not cause symptoms and require no surgery. If, however, these stones attempt to pass out of the gallbladder and block the gallbladder outlet, severe upper abdominal pain can develop.
Many patients have gallstones which do not cause symptoms and require no surgery. If, however, these stones attempt to pass out of the gallbladder and block the gallbladder outlet, severe upper abdominal pain can develop.
Common symptoms may include:
- Upper abdominal pain, occurring after meals rich in fat.
- Nausea and vomiting.
- Pain between the shoulder blades, and beneath the right shoulder.
- Chills and fever.
- Symptoms usually last for short periods of time and often occurs after fatty meals which stimulate the gallbladder to contract.
The formation of gallstones seems to be related to many factors, some of which are:
- Body weight - over-weight people have a higher incidence of gallstones.
- Diet - a diet high in fat and cholesterol, and low in fibre.
- Gallbladder motility - if the gall bladder is slow to drain.
- Rapid weight loss - bariatric surgery patients experience higher incidences of gallstones.
Acute Cholecistitis
Occasionally, these stones may become lodged within the neck of the gallbladder and result in prolonged episodes of pain associated with infection. This is known as acute cholesystitis and generally requires admission to hospital and cholecystectomy.
Obstructive Jaundice
Another complication of gallstones may be obstructive jaundice. In this situation, the gallstones pass out of the gallbladder and into the bile duct where they block the bile duct exit; that is, the gallstones prevent the flow of bile secretions into the duodenum. Jaundice is first recognised in the eyes, but acute jaundice results in a yellow tinge onto the skin. This may result in cholangitis, a progressive form of jaundice and infections. This needs to be treated immediately. Once a person has had one attack of gallstones, they are likely to develop more. It is thus wise to remove the gallbladder between attacks, since surgery is simpler when there is no acute infection or obstruction.
Treatment
A small hole (port) is created, in the belly button, followed by the insertion of a thin scope with a camera at its end to allow visualisation within the abdominal cavity. A second port is placed just under the breast bone, sternum, in the mid line of the abdomen, while third and fourth ports are placed in the right side of the abdomen. (These allow for removal of the gallbladder later in the procedure.).
The gallbladder is then freed of any scar tissue which may be present from previous episodes of acute cholecystitis. The cystic duct (the duct that joins the gallbladder to the bile duct) is then identified. Also identified is the cystic artery, a small blood vessel leading to the gallbladder.
The cystic duct is divided after sealing it with metallic clips. The cystic artery is then clipped and divided and the gallbladder is separated from the bed of the liver with a cautery device or laser. The gallbladder is then removed through one of the small incision ports. Finally, the ports are closed.
Patients are able to eat immediately after waking from a lap chole procedure and are usually discharged home the next day. Most patients return to normal activities within one to two weeks of their surgery.
The gallbladder is then freed of any scar tissue which may be present from previous episodes of acute cholecystitis. The cystic duct (the duct that joins the gallbladder to the bile duct) is then identified. Also identified is the cystic artery, a small blood vessel leading to the gallbladder.
The cystic duct is divided after sealing it with metallic clips. The cystic artery is then clipped and divided and the gallbladder is separated from the bed of the liver with a cautery device or laser. The gallbladder is then removed through one of the small incision ports. Finally, the ports are closed.
Patients are able to eat immediately after waking from a lap chole procedure and are usually discharged home the next day. Most patients return to normal activities within one to two weeks of their surgery.
Complications
Laparoscopic cholecystectomy has a complication rate of under two percent. It is a well-documented and frequently-performed procedure. Most patients recover and resume normal activities quickly. Rarely does the surgery impact adjacent organs in the body. When this occurs, a second procedure may be required.
Laparoscopic Gastrectomy
Overview
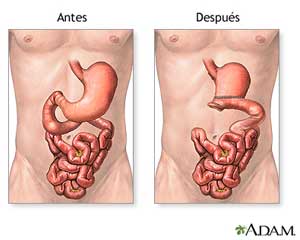 A gastrectomy is a procedure done to remove part or all of the stomach. When done using "keyhole" surgery it is called a laparoscopic gastrectomy. While the stomach is part of the digestive tract, with several lifestyle changes and the assistance of your doctors, you can still digest liquids and foods.
A gastrectomy is a procedure done to remove part or all of the stomach. When done using "keyhole" surgery it is called a laparoscopic gastrectomy. While the stomach is part of the digestive tract, with several lifestyle changes and the assistance of your doctors, you can still digest liquids and foods.
Indications
A laparoscopic gastrectomy is generally done as treatment for cancerous tumours in the stomach but may also be done to remove polyps, or growths inside your stomach or to treat severe stomach ulcers. There are three major types of gastrectomies: partial, complete and sleeve gastrectomies. Which of the above-mentioned types chosen by your surgeon will depend on your particular case.
What happens during a laparoscopic gastrectomy?
Under general anaesthesia a few small incisions will be made in the abdomen. Through these incisions a laparoscope, which is a thin surgical tool fitted with a camera and light, will be inserted. This provides your surgeon with images of the internal structures without the need for a larger incision. With this visualisation, Dr Heyns can remove part (a partial gastrectomy) or all (a complete gastrectomy) of the stomach as well as some nearby tissue like your lymph nodes.
Thereafter, depending on your specific case, your digestive tract will be rebuild accordingly. If a partial gastrectomy was done, the remaining part of your stomach will be connected to your bowel. If the entire stomach was removed your esophagus will be connected directly to your small intestine.
While Dr Heyns prefers the least invasive approach, this surgery can also be done through traditional open surgery.
Thereafter, depending on your specific case, your digestive tract will be rebuild accordingly. If a partial gastrectomy was done, the remaining part of your stomach will be connected to your bowel. If the entire stomach was removed your esophagus will be connected directly to your small intestine.
While Dr Heyns prefers the least invasive approach, this surgery can also be done through traditional open surgery.
What to expect after surgery
You can expect to stay in the hospital for one to two weeks after the surgery. While in hospital you will be fed through a tube in your vein until you are able to eat normally. Various lifestyle and dietary changes may need to be made but your doctor will discuss this with you prior to surgery. A dietician will then discuss your restrictions with food after surgery. Since laparoscopic surgery is less painful and allows for a quicker recovery time, you can expect to be back to your normal day-to-day routine in 3 weeks.
